Movement, activity and exercise benefit your overall health and wellbeing, improve your fitness, lift your mood and enhance your quality of life. Being able to move in a relaxed way and being physically active helps you do the things that are important to you; have fun, play sport, study, work or catch up with friends and family.
What and how you move and exercise is different for every young person with pain and there is no ‘one size fits all’ when it comes to activity and movement. This includes young people living with chronic conditions like Juvenile Idiopathic Arthritis or Chronic Widespread Pain, where movement, activity and exercise are key pain management strategies.
This following content describes how movement, activity and exercise can help re-train more normal communication between the body and the mind, and empower you to move confidently and do the things that are meaningful to you.
Movement is important for your health and a big part of managing your pain
What do we mean by “movement”? Movement refers to anything that involves moving your body – this is not limited to structured exercises (like doing a program at the gym). This can include walking to school or work, regularly changing your posture, relaxing or stretching, running and so on.
Movement and exercise have some excellent benefits for both pain and your overall health. Movement can help turn the ‘pain volume’ down, build your confidence, keep you active and doing things your love, and improve you sleep, stress levels, and mood. Movement is also really good for the health of your body, keeping you strong and agile even when you have pain.
There are a lot of myths about whether or not it is OK for young people with pain to exercise. Myths can be very unhelpful. Understanding what is true and what is false is the first step to understanding how movement and exercise can fit into your pain management plan.
In this video, young people share their experiences of myths and facts, helpful and unhelpful beliefs and messaging, ways to move more freely and confidently with pain and get back to valued life activities.
After an incident such as falling off a bike, you might expect to experience pain if you have taken skin off, bruised or scraped your arm or leg or broken a bone. Here, pain is expected, is normal and is important to help you recover from the acute tissue damage.
Tissues typically heal quickly and well and in the majority of cases, pain resolves.
Sometimes, pain can persist beyond the natural healing time (for acute injuries, usually 6-8 weeks). Sometimes pain can be experienced even when there is not an injury. This means your nervous system is hyper-alert, making you more likely to feel pain and be overprotective.
While this sort of pain can be puzzling, there is good science now to help make sense of why it happens. This is a bit like an oversensitive ‘alarm system’ and can be easily triggered.
The good news is there are helpful approaches to address pain that persists. The pain management modules in this website take you through these approaches.
"Find a way to move and exercise that works for you and your personal circumstance!"
Myths and facts that can help you understand more about moving safely with pain
Myth: Pain with movement is a sign of ongoing damage in the body
Fact: Pain can occur even when there is no tissue damage. Ongoing pain with movement, or pain with simple activities like walking and bending, is a sign that the body is sensitized to activity and not used to exercise or movement.
Myth: The body needs more attention /protection when pain is persistent
Fact: When you experience persistent pain, our brain can pay too much attention to the body and this is unhelpful. Engaging in graded activities (building little bits up gradually) that are fun, distracting, and physically active, helps retrain your system and build confidence.
Myth: When pain persists it means more rest is needed
Fact: Too much rest often makes pain worse; finding the ‘middle ground’ or ‘doings little bits often’ is more helpful and avoids pain flare ups. For young people with inflammatory conditions, managing both rest and movement is key.
Myth: Tensing the body during movement and holding ‘good’ posture is important to manage/avoid persistent pain
Fact: Relaxed movement and posture are important to manage your pain and helps restore your functional ability to do things that matter for you.
Myth: Activities that provoke pain should be avoided
Fact: Avoidance of movement and personally-important day-to-day activities can make persistent pain worse and impact your general wellbeing.
To learn more, check this module making sense of your pain.
What if it hurts when I move?
When you have pain, it can be hard to keep moving! Pain can get in the way of movement, activity and the exercise you enjoy. However, in most cases, moving with pain is beneficial, safe and necessary for your recovery.
You may feel like not moving to avoid pain (which means ‘underdoing’ activity), or moving differently (‘tensing up’); or ignoring pain and pushing on excessively (‘overdoing’ activity). This is understandable in the short term, but is unhelpful in the long run as pain takes control of what you do.
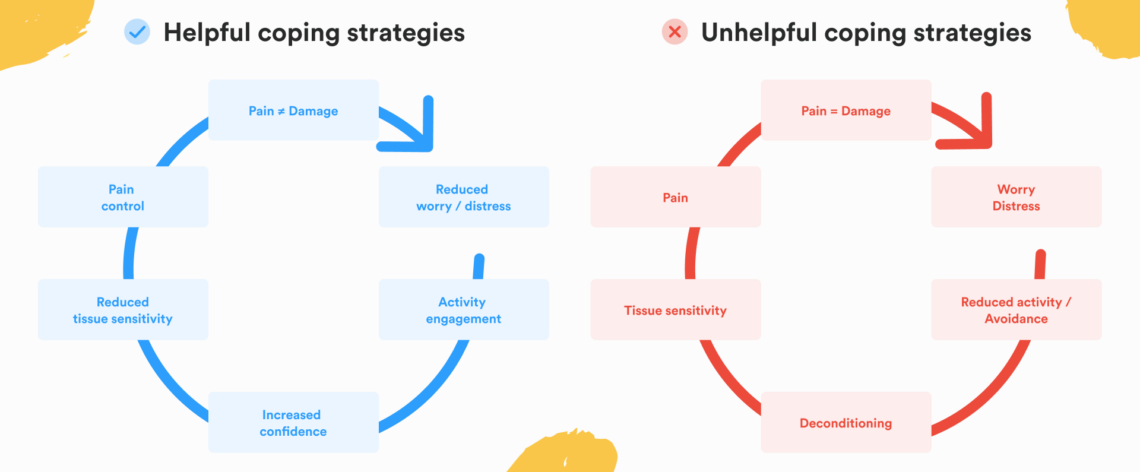
Below you’ll see a graphic showing on the left-hand side what an unhelpful approach to pain looks like – this is common. On the right-hand side, you can see how changing what how you think about pain, can provide a different helpful way to manage pain safely, build your confidence and put you back in control.
Factors that can influence your decision to move, be active and exercise when you have pain
What are my beliefs about pain? Beliefs about pain influence what you do.
For example, a helpful belief is ‘experiencing some pain during movement and exercise is part of recovery and does not mean I am causing more damage; it is safe to move’). Here, you are more likely to engage with movement and exercise and improve recovery. Believing that pain during exercise means causing harm to my body; more hurt means more harm; I am doing more damage; It is not safe to move), then it is much harder to engage with movement and exercise, and your recovery is likely to be slower. Learning how to safely move is key here along with dispelling unhelpful myths.
What are the beliefs of the people taking care of me?
Consistent advice from your ‘healthcare team’ to start moving and exercising in a graduated manner, with clear instruction and guidance is some of the best advice you can get! See making sense of your pain to learn more about how a health care team can best support your recovery. If your health team has positive beliefs about the importance of safe movement with pain, they are likely to support you engaging with movement and exercise and this can positively impact your recovery. Unhelpful beliefs from your team about pain (things like pain means damage, or pain means you must always rest), can negatively impacts your recovery.
How do I respond when I feel pain, or when I think a movement will hurt?
Your responses to pain or in anticipation of pain can influence your recovery. Thoughts about pain (for example, pain means damage/more harm), thinking the worst about pain or excessively worrying (e.g. this pain will never go away) magnifies the danger of pain, the brain goes on alert and normal movements become overly protective. This can increase the feeling of helplessness about pain, lowering our mood and leaving you feeling frustrated. If you recognise these responses, then talk to your healthcare team and ask for some help and strategies to support moving more normally, being active and exercising. Check out approaching pain management module and the mindfulness and pain for practical ways to better manage your pain.
Do I feel scared about pain?
It’s really normal to experience some fear when you have pain. You might stop moving or tense up when you move because of pain. You might think this pain is doing more damage. Remember, experiencing some pain with movement is normal in the recovery journey. When you are scared to move, this is commonly associated with tensing up or clenching the muscles around the painful body part. For example, in young people with back pain, you might tense up the back and belly muscles when you move or hold your breath). This response is understandable but can slow your recovery. It is important to discuss these fears with your health professional and get some practical tips to help you get moving safely.
Do I understand what pain means when I move or exercise?
Remember that pain is a sign that your body/systems are sensitive and getting used to moving and exercising again. This does NOT mean that you should push through pain (‘overdo’). Pushing through pain can lead to a ‘yo-yo’ cycle of pain, rest and inactivity. While pain during movement and exercise is normal, finding a balance between overdoing and underdoing is key. Finding the middle ground and moving more in a graduated way is the best approach. You may need some coaching from a healthcare team to go through this process. See our making sense of your pain or getting back to what you want to do modules for more info.
Do I know where my body is in space?
In some conditions, like low back pain and Complex Regional Pain Syndrome), persistent pain can affect your body’s inbuilt GPS tracking system…you can feel like your body is ‘lost in space’. You may feel that you are sitting relaxed, but when you look in the mirror, you are sitting bolt upright and your back is not even touching the backrest. Body and mind re-training to re-orient your body in space or “restore your GPS” is possible. Our natural capacity for learning relates to Neuroplasticity (i.e. brain’s ability to learn new tricks), Using neuroplasticity can be part of managing pain. Ask your health professional about this re-training approach.
I have Juvenile Idiopathic Arthritis, is safe for me to exercise?
Exercising with Juvenile Idiopathic Arthritis is safe; your joints get healthier with graduated movement and exercise. Exercise is also good for your overall health, including your heart, lungs, immune system, brain, and mood. If you have Juvenile Idiopathic Arthritis, managing pain flares and activity is key. Check with your rheumatologist to see if your medications are right for you, so you can keep moving safely – the type of medication and/or the dose may need tweaking. If you experience a pain flare, it is not recommended to push through this, but talk to your care team for advice. Taking more rest breaks, and learning how to get back to what you want to do is usually helpful. To learn more about Juvenile Idiopathic Arthritis, check out our Juvenile Arthritis

Understanding the body-mind relationship and how it influences your habits, including movement and exercise, is very important in making sense of your pain and how to manage it. For some young people who experience intrusive thoughts and challenging beliefs around pain, working with both a Clinical Psychologist and a Physiotherapist with experience in managing pain holistically, can be more effective than working with just one or the other.
"Family and friends can make a big difference to young people’s experience of pain"
Is there a right type of exercise for you? Tips to help guide your exercise choices
The important thing is that the movement/activity and exercise plan is tailored to you and your own personal situation and interests. Movement and exercise need to match your needs and goals, and be realistic so you can build up over time: small gains become longer term wins.
Discuss your specific needs and condition with your physiotherapist, doctor or health professional to get the best movement/activity and exercise program to help you back to doing the things that matter. Here are some factors to discuss to help guide your movement/activity and exercise choices:
- Movement/activity and exercises that are ‘good for your health’ like walking, cycling or possibly swimming can be done by most young people with pain conditions. Walking is easy, free and can be done anywhere, anytime, alone or with friends and family or a dog. The choice will depend on what you like, what you have access to and what is the most appropriate for your pain problem.
- Movement/activity and exercises to train relaxed movement is vital. A relaxation and stretching program (tai chi, yoga or simple stretching and breathing) will benefit most young people. This is a good approach, if you experience stiffness and pain with movement or experience high levels of stress, anxiety or distress, or have difficulty with sleep.
- Movement/activity and exercises to improve the health of a body region (like lower limbs, upper limbs, spine) need to be tailored to you. Depending on your pain condition, you may need to be taught different (and more helpful) ways to move. You may need to strengthen specific muscles so you can walk for longer, swim for longer, jog or dance. For example, if you have a knee pain problem, you may benefit from exercises tailored to building your thigh and leg muscles, as these improve the strength and health of the joint.
- Exercises to improve balance and agility may be an important part of your exercise program. Building balance and agility can help build your confidence in using your body in more challenging situations. Tai chi or yoga are good options and can be done gently and safely.
- ‘Do’s and do nots’ depending on your condition. Sometimes, the wrong movement/activity or exercise program can create a pain flare. For example, if you are living with Juvenile Idiopathic Arthritis, it is important that your plan is appropriate for you, with the right dose of rest and movement/activity/exercise. If you have back pain and find yourself tensing the muscles around your spine, deep breathing and relaxing with movement can be helpful. However, in this same case ‘core strengthening’ exercises that are often recommended, can actually increase your pain.

Getting started with movement and exercise
Step one: Finding the right time to start moving
There’s never a ‘right time’ to start regular movement, exercise and activity. There’s often an excuse or reason to put it off. Pain is likely the most obvious reason. Remember, experiencing some pain during movement, activity and exercise is a normal part of managing pain and living well.
At times, it’s hard to have to DO something yourself to get moving. It’s good to remember to be kind to yourself. Go slowly, take small gains and keep your focus on longer term wins. Managing your pain using this approach places YOU in charge. Finding a health team to support you through and help you when needed, is key.
Remember that movement, activity and exercise is just one of the key pieces of your pain management plan. You can check out more info in our making sense of your pain module.
Step two: Taking up the challenge of moving with pain
Start slow Moving and exercising when you are in pain is not an easy task. Depending on your pain condition, you may be able to start working on movement and exercise by yourself, by simply using the advice presented here; or you might need to see a healthcare professional such as a physiotherapist or exercise physiologist to guide, support and ‘coach’ you.
Support along the way Not feeling alone can help in getting moving. Asking friends and family for support is a good plan. Organising an activity ‘date’ (walk, bike ride, swim etc.) once or twice a week with friends can help motivate you while having fun. See Shaun’s story, that is exactly what he did! A group exercise class that you’d found might be a good option and enjoyable. Check out the module on helping others help you.
Doing little bits often If you’re new to exercise (or haven’t done it for a long time) it’s a good idea to consider a pacing strategy. Pacing helps you break activity into smaller bits; doing little bits often or finding the middle road between not overdoing or under doing activity. Pacing keeps you active while avoiding pain flares. Although pain flares are common and do not mean you are causing more damage, they can slow your progress, so it’s good to know how to prevent this.
Your pacing strategy should include a plan to gradually increase the amount you can perform an activity over time. This allows your body time to get used to the new activity and build your confidence, strength and endurance, and reduce your body’s sensitivity to movement. For example, you may only be able to manage 10 minutes of continuous walking. Your goal may be to achieve 30 minutes of walking. To do this, you increase the amount you walk by 10% per week until you reach your goal of 30 minutes. The getting back to what you want to do module gives you practical guidance and tools.
Building strength and condition If you’re interested in building your strength and conditioning using weights, this is best done with a health professional with this expertise; a physiotherapist or exercise physiologist. Getting the correct type and dose of exercise (frequency, intensity, and duration), helps support you to gradually and safely build up your strength and confidence over time.
You can do this! To start moving and exercising when you are in pain, takes effort, courage and commitment. Be kind and gentle to yourself along the way and choose a daily, ‘good for your health’ activity or exercise you like. Regular activity and exercise are a great way to re-build confidence in your own body and better manage your pain and wellbeing.
Have you had a bad experience before with movement, activity and exercise? Try not to give up. A good skilled health professional with expertise can work with you to help tailor a plan to your needs and coach you.
Step three: What can I expect when I start exercising?
But my body is sore When you start movement, activity and exercising, it’s very common for your body to be a bit sore and/or stiff for a little while. Think of this as a ‘positive’, body re-training response. It is your body’s way of saying “Hey! I see what you are doing”. This is normal. As you keep moving and exercising regularly, the body will adapt and often say, “I remember now; moving and exercising is safe. Keep at it”.
How do I know it’s safe to move and exercise? Movement, activity and exercise is safe, it just needs to be done at the right amount and intensity (dose) to allow your body and mind time to adapt. As the muscles and mind get used to the activity or exercise, this soreness/pain/sensitivity reduces and muscles and joints build tolerance and strength. Soreness or sensitivity is usually more noticeable on the muscles around the painful body area, because they are usually the most unfit.
My pain has increased You might experience an increase in pain over a few hours or a day or two when you exercise; this is called a pain flare. This is very common and while it can be scary, it’s important to know that this does not mean you are doing damage! A pain flare is normal when starting a new activity or exercise program, as it takes a bit of time for your body to adapt. To reduce the occurrence of pain flares, try and make sure that you’re relaxed when you move or exercise. Taking a gradual and paced approach (regular with small increments over time) is really important.
Overdoing and underdoing A paced approach helps you to avoid overdoing or underdoing exercise and activity. If you know you are an “over-doer”, or try to push through your pain, before starting your new activity or exercise plan, try speaking with your physiotherapist or exercise physiologist. You can also check out our getting back to what you want to do module. This explains how you can set a baseline and get moving safely without causing a major pain flare. Progressing your exercise and activity using this approach, allows you to keep moving safely through a pain flare.
If you know you are an “under-doer” and you are afraid to move and exercise, you may not be doing enough (dose is too low). If there is no benefit, you might think that exercise doesn’t work for you. Getting the right guidance can help to get on track, do enough safely and stay on track. Finding a health professional with exercise expertise to coach your through the start of an exercise program, at the right dose and frequency can make all the difference to your recovery.
Step four: Urges to stop
Should I stop when I am in pain? People in pain are often told to stop moving and exercising if they feel pain; or, to only progress the exercise once pain stops. Most times, this is unhelpful.
Tracking how long you can do the exercise for works well here – what is called a time-contingent approach or pacing. This means you keep going with movement or exercise even when you have pain. Then, you gradually increase this activity or exercise about 10% each week based on time and your goals rather than based on pain.
For young people with conditions where fatigue is a problem such as Juvenile Inflammatory Arthritis or Chronic Widespread pain, pacing activity with appropriate rest periods for recovery, will be important. Time and dose is especially important for young people with these conditions and require skilled advice to support careful tailored planning that works best for you.
Small wins mean longer term gains Like any new habit that requires us to commit and do the “hard yards”, there will be times when you don’t want to exercise! Continuing regular movement, activity and exercise, moving often and maintaining activities will help you to stay engaged and connected socially. Be kind with yourself and plan for these tough times. You may also like to take a friend with you, or the dog to help motivate you to keep up with your program.
Tracking progress Keeping a diary either handwritten or by using e-tools like ‘Apps’ (available through iTunes) for your smart phone and devices (e.g. iPhone/iPad) can help log your activity and exercise progress. Many Apps are free and allow you to log your daily exercise, your energy expended and some even have GPS tracking to allow you to measure how many steps you take, distance travelled or time taken. You may find it helpful to have your health professional, a family member or friend use smart devices (iPhone/iPad or Smart Phone) to video you every few weeks, so you can see your progress (e.g. your flexibility).
Want more information?
Here are some helpful apps and websites to help you track your pain and set goals to increase you level of physical activity. Alternatively, if you want to talk to someone, please seek further assistance.
Related management modules
References
- Kuntze, G., C. Nesbitt, J. L. Whittaker, A. Nettel-Aguirre, C. Toomey, S. Esau, P. K. Doyle-Baker, J. Shank, J. Brooks, S. Benseler and C. A. Emery (2018). Exercise Therapy in Juvenile Idiopathic Arthritis: A Systematic Review and Meta-Analysis. Arch Phys Med Rehabil 99(1): 178-193.e171. [PubMed]
- de Zoete, R. M. J., L. Brown, K. Oliveira, L. Penglaze, R. Rex, B. Sawtell and T. Sullivan (2020). The effectiveness of general physical exercise for individuals with chronic neck pain: a systematic review of randomised controlled trials. European journal of physiotherapy 22(3): 141-147. [T&F Online]
- Slater, H., J. E. Jordan, J. Chua, R. Schütze, J. D. Wark and A. M. Briggs (2016). Young people’s experiences of persistent musculoskeletal pain, needs, gaps and perceptions about the role of digital technologies to support their co-care: a qualitative study. BMJ Open 6(12): e014007. [BMJ Open]
- Slater H, Jordan JE, Chua J, Schütze R, Briggs AM (2016): Young people’s experiences of living with persistent pain, their interactions with health services and their needs and preferences for pain management including digital technologies. Melbourne: Arthritis and Osteoporosis Victoria and Arthritis and Osteoporosis Western Australia. [Arthritis WA]